INTRODUCTION
Mechanisms that determine the morphometric proportion of various human body parts during embryogenesis are largely unknown. Physiological variations in the dimensions of body parts are well known not only between but also within, different races. Macrodactyly, congenital hemihypertrophy, and Proteus syndrome are some examples of organ overgrowth that defy the control mechanism. Herein, a newborn, which is thought to have an abortive overgrowth of the fronto-nasal process during embryonic life, is reported.
CASE REPORT
A 3-day-old term gestation male newborn, first-order birth born of non-consanguineous parents was admitted to the Department of Pediatric Surgery at Madurai Medical College because of a congenital mass hanging from the tip of the nose. His mother was not exposed to any of the known teratogens during gestation. There was no history of birth asphyxia. There were no malformations of the other organ systems.
Clinical examination revealed a pedunculated bi-lobed mass of 2 x 1 x 1 cm arising from the right border of the nasal columella. A deep groove did separate the two symmetrical lobes (Fig. 1). The mass was soft with a few areas of firm consistency. There was no intranasal extension of the mass, with the normal nasal septum. Its surface was covered with wet mucosa. Its pedicle was 4 mm wide and 1 cm long. Upper lip, nasal tip, and ala, palate and face were otherwise unremarkable. Biochemical and hematological investigations including serum alpha-fetoprotein were within normal limits. A Computerized Tomography scan of the skull was a normal study. On the sixth day of life, the mass was excised by snaring the pedicle. On follow-up after 6 months, the child was asymptomatic and the growth of the nose was satisfactory.
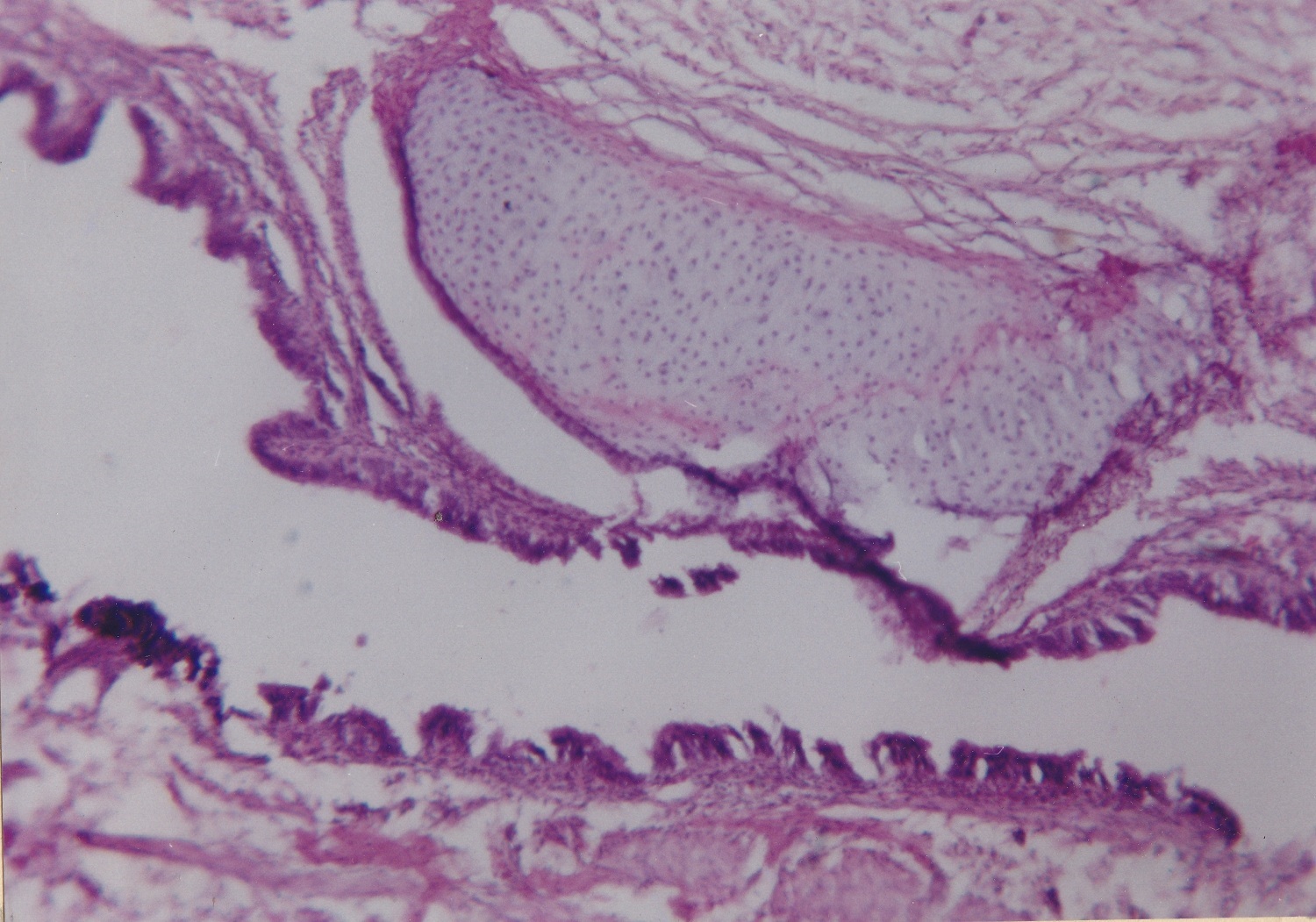
The cut section of the mass was homogenous, fleshy and there were a few areas of firm consistency. Histopathology of the mass revealed ciliated columnar epithelium, cartilaginous tissue, few blood vessels, and connective tissue stroma (Fig. 2). Multiple section studies using silver and PAS stains did not show any neural elements or other ectopic tissues.
DISCUSSION
Congenital masses arising from the nose are extremely rare with an incidence of 1 in 20000 or 1 in 40000 live-births.[1] Nasal tip masses are still rarer. The list of differential diagnoses of congenital nasal mass commonly includes encephalocele, glial heterotopias of the nose, midline dermoid, nasal chondromesenchymal hamartoma (NCMH), hemangioma, rhabdomyosarcoma, teratoma, neurofibroma, and nasolacrimal duct cyst.[2] Teratomas, nasal gliomas (glial heterotopia), and hamartoma are the congenital lesions that are reported to occur in the tip of the nose. There are only 3 cases of nasal tip teratomas reported in the literature.[3], [4], [5] Teratoma by definition should contain derivatives of all three embryonic germinal layers and the tissue should be foreign to the area. In the present case, ciliated epithelium represents ectodermal derivative while cartilage represents mesodermal derivative, but none of them are foreign to the nose. Hence, teratoma would be an incorrect diagnosis. During development, a portion of the forebrain may get detached and become adherent to the nose before the closure of the skull base. Such heterotopic brain tissue in the nose is well known as Nasal Gliomas.[6] However, the absence of neuroglia in histology excludes this possibility in our case. Nasal chondromesenchymal hamartoma described by McDermott in 1998 is a rare lesion that has been reported more than 38 times since then.[7], [8] Such hamartomas are never bi-lobed. Therefore we believe that our case is unique and is possibly a new disease entity.
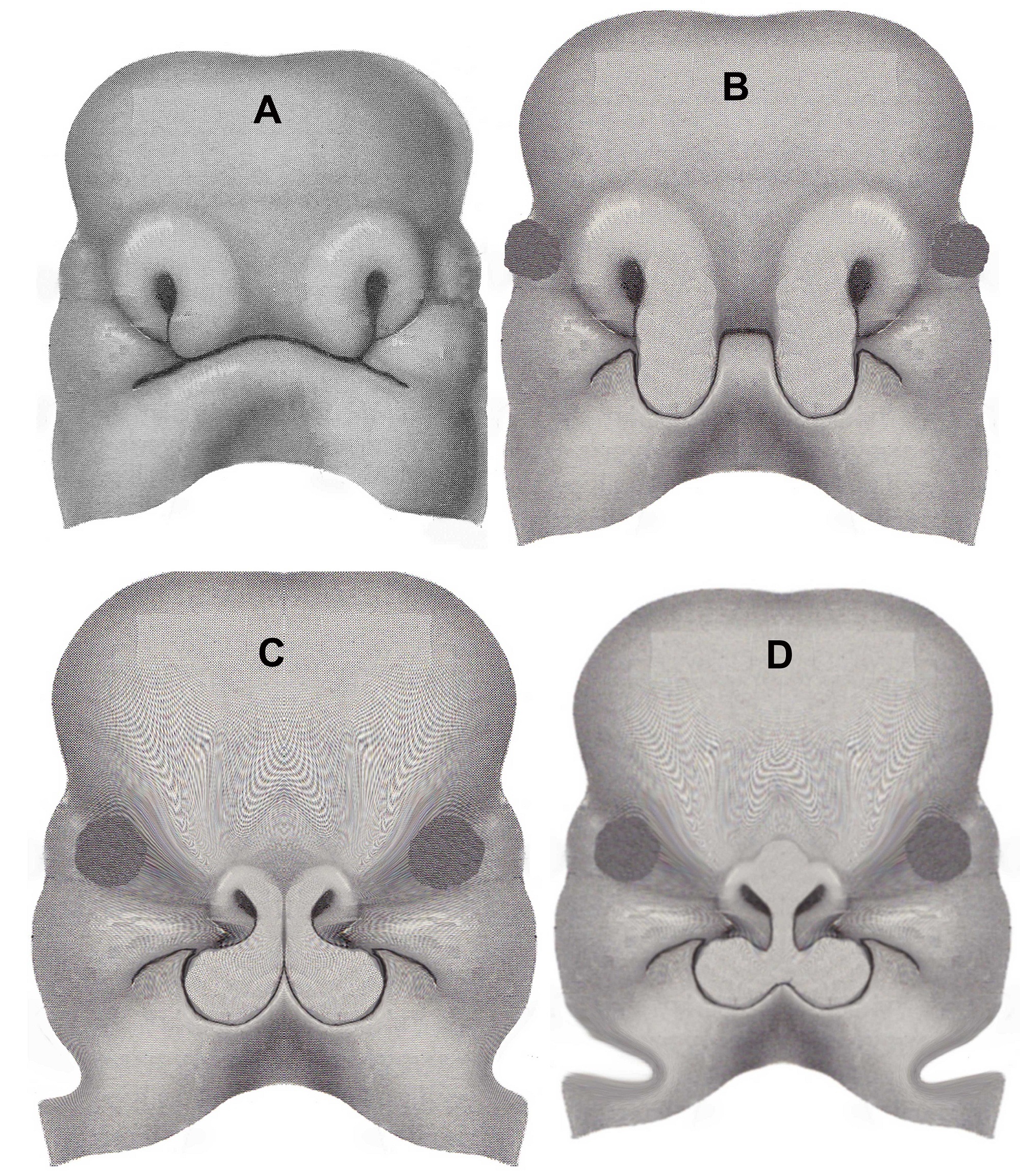
We hypothesize that our case may be explained by the embryonic overshoot of nasal development. The nose develops from the frontonasal process which becomes medial and lateral nasal processes. The fusion of the medial nasal process forms the septum and the nasal tip. Regional organizer cells induce differentiation of nasal tissues and direct the development of the fronto-nasal process.[9] These embryonic processes stop elongating after reaching the predetermined level thereby determining the characteristic length of the nose in each individual. The exact mechanism that controls this process is not yet identified, but it could be genetic cell signaling. This is evident from the characteristic length of the nose in different races. A defect in the control mechanism during development could possibly result in overshooting of the nasal processes. This hypothesis explains the pathogenesis of our case (Fig. 3). The bi-lobed nature of the mass suggests that it could have developed from the fusion of two medial nasal processes. Further research is needed to unravel the mystery of such lesions and it will broaden our understanding as to how various body proportions are embryologically determined.
Notes
n1Conflicts of interest. None
n3Author contributions: Author(s) declared to fulfill authorship criteria as devised by ICMJE and approved the final version. Authorship declaration form, submitted by the author(s), is available with the editorial office.
n4Consent to Publication: Author(s) declared taking informed written consent for the publication of clinical photographs/material (if any used), from the legal guardian of the patient with an understanding that every effort will be made to conceal the identity of the patient, however it cannot be guaranteed.
References
|
|
| 1. |
Kennard CD, Rasmussen JE. Congenital midline nasal masses: diagnosis and management. J Dermatol Surg Oncol. 1990; 16:1025-36. |
| 2. |
Wang IJ, Lin SL, Tsou KI, Hsu MC, Chiu WT, Tsai SH, et al. Congenital midline nasal mass: cases series and review of the literature. Turk J Pediatr. 2010; 52:520-4. |
| 3. |
Shetty SC, Gupta S, Cherian M, Chary G, Sharif S. Mature teratoma of the nasal vestibule: a case report. Ear Nose Throat J. 2000; 79:620-3.
|
| 4. |
Benacerraf BR. Picture of the mouth. A nasal tip teratoma. Ultrasound Obstet Gynecol.1999; 14:22.
|
| 5. |
Hansen M, Schofeild DE, Benacerraf BR, Mulliken TB. Large nasal Tip teratoma. Ann Plast Surg. 1995; 35:522-4.
|
| 6. |
Pereyra-Rodríguez JJ, Bernabeu-Wittel J, Fajardo M, Torre C, Sánchez-Gallego F. Nasal glial heterotopia (nasal glioma). J Pediatr. 2010; 156:688.
|
| 7. |
Hsueh C, Hsueh S, Gonzalez-Crussi F, Lee T, Su J. Nasal chondromesenchymal hamartoma in children: report of 2 cases with review of the literature. Arch Pathol Lab Med. 2001; 125:400-3.
|
| 8. |
Norman ES, Bergman S, Trupiano JK. Nasal chondromesenchymal hamartoma: report of a case and review of the literature. Pediatr Dev Pathol. 2004; 7:517-20.
|
| 9. |
Donner AL, Williams T. Frontal nasal prominence expression driven by Tcfap2a relies on a conserved binding site for STAT proteins. Dev Dynamics. 2006; 235:1358–70.
|