Introduction
Teratomas are relatively common in childhood, with an incidence of approximately 1 in 4,000 live births.[1] While most teratomas occur in the sacrococcygeal region, craniocervical teratomas, including oral teratomas, represent a small percentage, comprising only 2-5% of childhood teratomas. [2]
Oral teratomas pose unique challenges in achieving complete resection and ensuring favorable functional and cosmetic outcomes. [3] Also known as epignathus, oral teratomas primarily develop in the sphenoid region, specifically on the palate or pharynx, referred to as Rathke's pouch. [4] Rarely, they may be found in the nasal cavity of the hard palate. This case report presents a rare occurrence of an oral teratoma attached to the palate and extending sublingually on the right side, accompanied by a cleft palate.
Case Report
A male baby was delivered via cesarean section- due to oligohydramnios and the presence of a large oral mass- at 39 weeks to a 29-year-old mother and 38-year-old father. The baby weighed 3200 g at birth, and the APGAR scores were 7 and 8 at 1 and 5 minutes, respectively. On the 16th day of life, the patient was referred to the pediatric surgery department with an initial diagnosis of heteropagus twins.
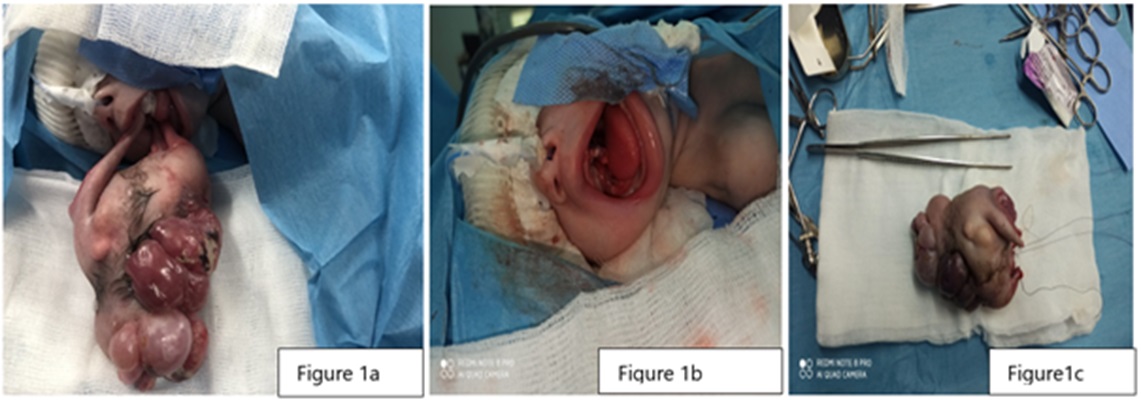
Upon craniofacial examination, plagiocephaly and a mass measuring 72mm x 44mm were observed. The mass was attached to the palate, extending sublingually on the right side, and a cleft palate was also present (Fig. 1). The child's hemogram was normal, and serum levels of alpha-fetoprotein (AFP) and beta-human chorionic gonadotropin (b-HCG) were within the normal range for their age.
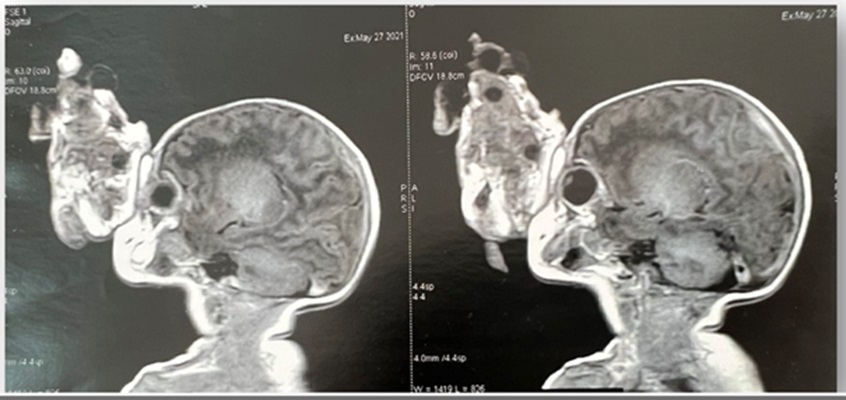
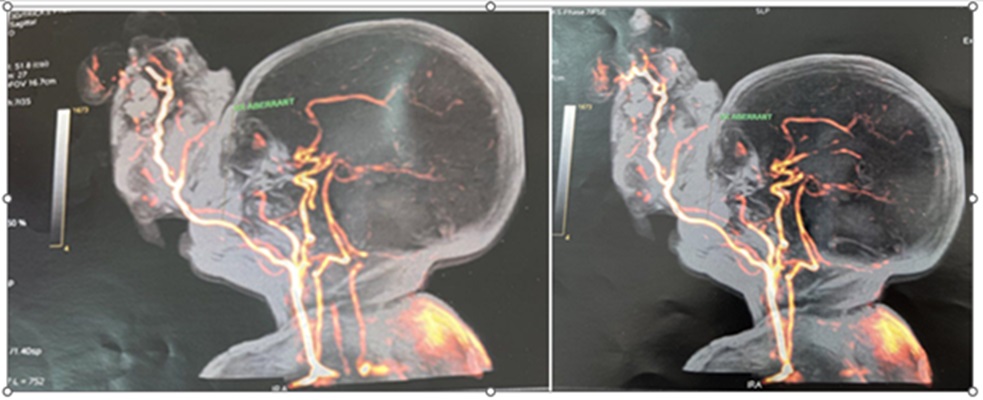
The mass was heterogeneous having bony structures and a soft cystic component. Computed tomography (CT) revealed a large facial mass protruding through the mouth, consisting of central calcific components, peripheral fat, and a solid cystic component without any intracranial extension (Fig. 2). Facial angio-magnetic resonance imaging (MRI) showed a mass with three endo-buccal pedicles inserted into the right oropharyngeal wall, partially filling the nasopharynx. Arterial vascularization originating from the ipsilateral carotid vessels was observed, along with an aberrant vessel measuring 2.5 mm in diameter extending to the distal part of the mass (Fig. 3). Abdominal ultrasound, echocardiogram, and ECG results were all within normal limits.
The surgical procedure, performed on the 17th day of life, involved complete excision of the teratoma. The histopathology report confirmed the presence of a mature tridermal teratoma with various tissue components, including skin covering, salivary glands, bronchial epithelium, cartilage, and glial tissue. The patient experienced a smooth postoperative course, with only a residual ovoid mass measuring 2 cm x 0.5 cm observed in the right oropharynx. A second operation was performed at 6 months to remove the residual mass, and the cleft palate closed at 18 months. Currently, two years after the surgery, the child is in good health.
Discussion
Oral teratoma may exhibit a potential for airway obstruction in newborns which is a significant challenge that may require immediate medical attention.[5] Given the rarity of oral teratomas, their specialized management becomes pivotal for effective care. Early prenatal diagnosis through ultrasound screenings is a noteworthy advancement, facilitating timely intervention and specialized care planning after birth [6]. Notably, certain cases of oral teratomas are linked to cleft palate, particularly when the tumor develops early during gestation [7].
The recognition that oral teratomas may be associated with heteropagus twins or incomplete conjoined twinning adds complexity to understanding these tumors. This report underscores the importance of distinguishing between the two conditions based on the presence or absence of a spinal column. [8]
The treatment of oral teratomas necessitates meticulous surgical planning to ensure complete excision while preserving vital structures, especially when the tumor extends into the oropharyngeal wall. The likelihood of post-tumor removal remodeling and the presence of residual masses may require subsequent surgical interventions and comprehensive follow-up care. Similarly in the index case, the residual tumor was excised at 6 months.
The management strategies include promoting early prenatal diagnosis, [9] fetal intervention where necessary, birthing the baby in a specialized center, and collaborative efforts to excise such tumors by anesthesiologists, neonatologists, and pediatric and fasciomaxillary surgeons. [10] Utilizing imaging modalities such as computed tomography (CT), magnetic resonance imaging (MRI), and angiography is crucial for evaluating tumor characteristics and aiding in surgical planning, ensuring procedural safety. We too used these modalities for better planning of the excision. In addition to the tumor markers of teratoma, histopathological examination is important for precise diagnosis, as malignant lesions will need chemotherapy in addition to surgical resection.
Oral teratomas are rare congenital tumors that require early prenatal diagnosis, immediate intervention after birth, and specialized care from a multidisciplinary team. Successful management involves addressing associated anomalies and providing comprehensive healthcare to ensure favorable outcomes for the patient.
Notes
n1Conflicts of interest. None.
n3Author contributions: Author(s) declared to fulfill authorship criteria as devised by ICMJE and approved the final version. Authorship declaration form, submitted by the author(s), is available with the editorial office.
n4Consent to Publication: Author(s) declared taking informed written consent for the publication of clinical photographs/material (if any used), from the legal guardian of the patient with an understanding that every effort will be made to conceal the identity of the patient, however it cannot be guaranteed.
References
|
|
| 1. |
Koné FI, Hajjij A, Cissé N, Soumaoro S, Wahabhaidara A, Timbo SK, et al. Congenital cervical teratoma. Surg Sci. 2019; 10:44–8. Available from: https://doi.org/10.4236/ss.2019.101006. |
| 2. |
Paradis J, Koltai PJ. Pediatric teratoma and dermoid cysts. Otolaryngol Clin North Am. 2015; 48:121-36. Available from: https://doi.org/10.1016/j.otc.2014.09.009. |
| 3. |
Peterson CM, Buckley C, Holley S, Menias CO. Teratomas: a multimodality review. Curr Probl Diagn Radiol. 2012; 41:210–9. Available from: https://doi.org/10.1067/j.cpradiol.2012.02.001.
|
| 4. |
Kadlub N, Touma J, Leboulanger N, Garel C, Soupre V, L’Herminé AC, et al. Head and neck teratoma: From diagnosis to treatment. J Craniomaxillofac Surg. 2014; 42:1598-603. Available from: https://doi.org/10.1016/j.jcms.2014.04.028.
|
| 5. |
Brodsky JR, Irace AL, Didas A, Watters K, Estroff JA, Barnewolt CE, et al. Teratoma of the neonatal head and neck: A 41-year experience. Int J Pediatr Otorhinolaryngol. 2017; 97:66-71. Available from: https://doi.org/10.1016/j.ijporl.2017.02.011.
|
| 6. |
Feygin T, Khalek N, Moldenhauer JS. Fetal brain, head, and neck tumors: prenatal imaging and management. Prenat Diagn. 2020; 40:1203-19. Available from: https://doi.org/10.1002/pd.5722.
|
| 7. |
Dakpe´ S, Demeer JR, Cordonnier C, Devauchelle B. Emergency management of a congenital teratoma of the oral cavity at birth and three-year follow-up. Int J Oral Maxillofac Surg. 2014; 43:433-6. Available from: https://doi.org/10.1016/j.ijom.2013.09.004.
|
| 8. |
Niedzielski A, Marciniak A, Mickiewicz M, Mielnik-Niedzielska G. Pharyngeal teratomas in children. J Pediatr Surg Case Rep. 2020; 54:101395. https://doi.org/10.1016/j.epsc.2020.101395.
|
| 9. |
Wolter NE, Siegele B, Cunningham MJ. Cystic cervical teratoma: a diagnostic and management challenge. Int J Pediatr Otorhinolaryngol. 2017; 95:97-100. https://doi.org/10.1016/j.ijporl.2017.02.016.
|
| 10. |
Kontopoulos EV, Gualtieri M, Quintero RA. Successful in utero treatment of an oral teratoma via operative fetoscopy: case report and review of the literature. Am J Obstet Gynecol. 2012; 207:e12-5. Available from: https://doi.org/10.1016/j.ajog.2012.04.008.
|