Introduction
Spontaneous pneumothorax has an incidence of 1-2% in term neonates and 6% in premature infants presenting with respiratory distress. [1] Pneumothorax can also be a complication of ventilation (3%), continuous positive airway pressure (CPAP) (9%), and endotracheal tube (ETT) insertion due to potential hypopharyngeal injury. [2] Subsequent hypoxia and hypercarbia lead to high morbidity and mortality (30%). [2] A massive air leak may manifest as pneumomediastinum and pneumoperitoneum. Pneumoperitoneum in a preterm neonate usually arises due to gastrointestinal perforation, mostly secondary to necrotizing enterocolitis.[3] Non-surgical pneumoperitoneum could occur due to a pulmonary air leak and may not require drains or laparotomy. [3] We herein report a case of a male preterm baby with a presumed iatrogenic airway injury.
Case Report
A baby boy (twin) was born at 28+3 weeks of gestation, to a 33-year-old mother. Due to cord prolapse, an emergency lower segment cesarean section was undertaken. APGAR scores were 2, 6, and 8 at 1, 5, and 10 minutes, respectively. Spontaneous respiration was attained after 4 minutes of the bag and mask inflation breaths. Due to apneic episodes on CPAP, he was intubated using a size 3 ETT with conventional ventilation at a peak pressure of 24 cmH2O and positive end-expiratory pressure (PEEP) of 5 cmH2O. Surfactant was administered. Chest radiography (CXR) showed increased left lung opacity and low-lying ETT tip. This was withdrawn for effective ventilation.
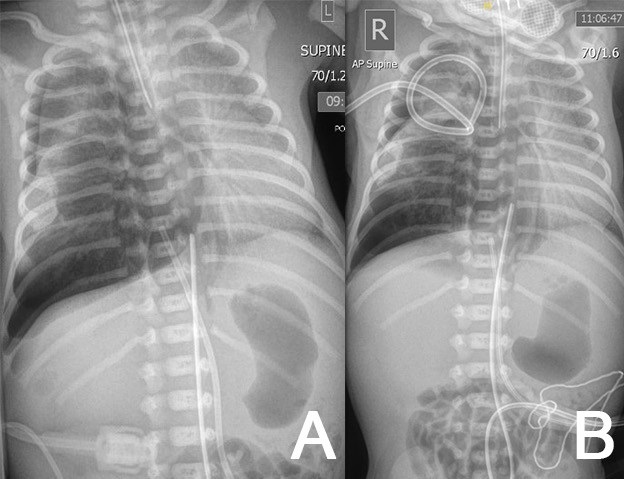
At 3 hours of age, due to sudden loss of chest movements and volumes on ventilation, the neonate was re-intubated. There was ongoing respiratory distress and CXR confirmed a right-sided tension pneumothorax (Fig. 1A). Needle aspiration followed by tube thoracocentesis (TT) with the underwater seal was undertaken (Fig. 1B) . The drain was placed on low-flow suction. One hour later, further desaturation and transillumination indicated a large residual pneumothorax, necessitating a second chest drain, also placed on low-flow suction. Ventilation improved and he remained on 25% FiO2.
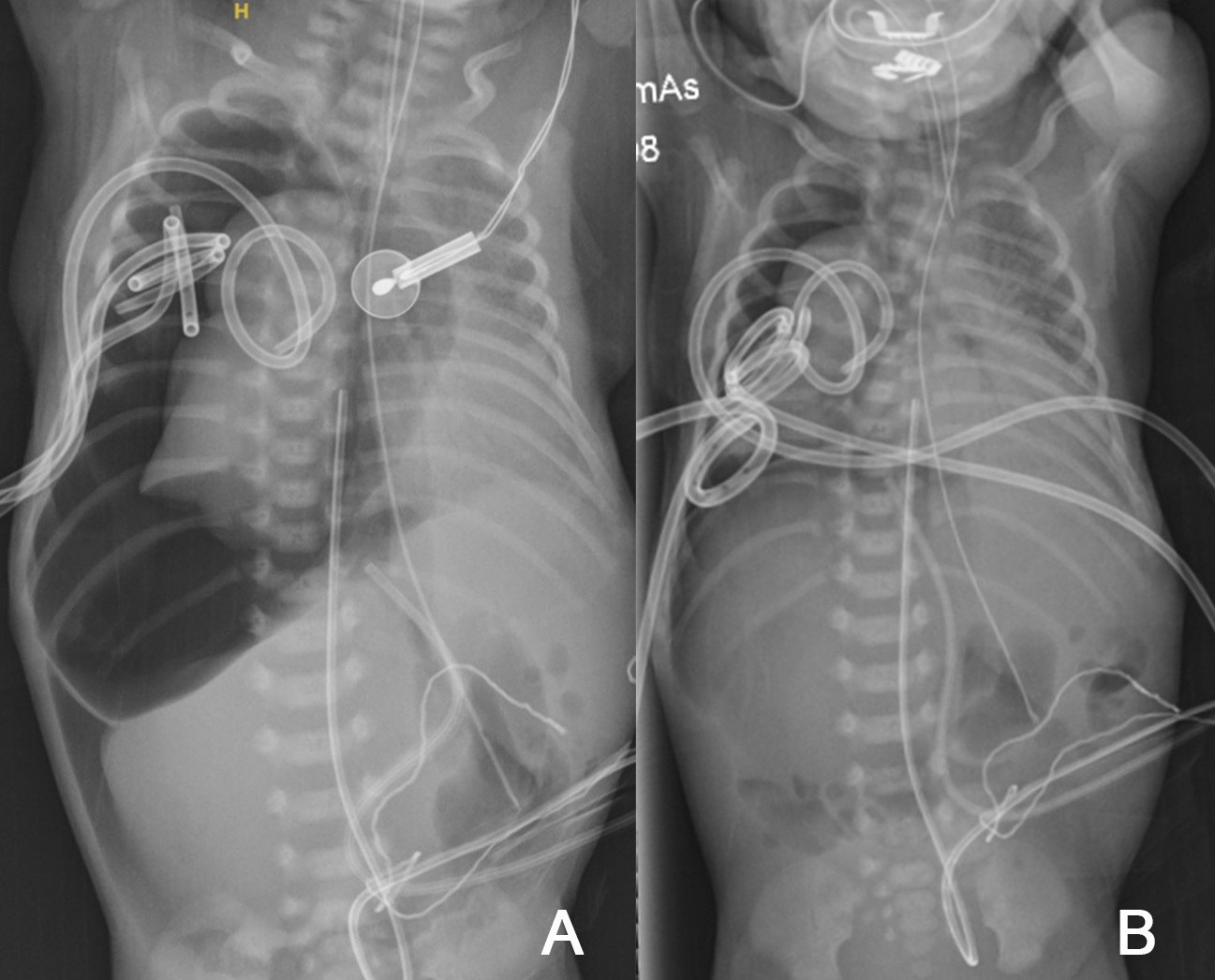
An iatrogenic tracheobronchial injury was suspected. On day 2, he developed a greater oxygen requirement; transillumination and radiography confirmed persistent pneumothorax, this time with pneumomediastinum and pneumoperitoneum, requiring a third chest drain. He was then transferred to the regional pediatric center. After a fourth TT (Fig. 2B) due to a massive ongoing air leak (Fig. 2A), high-frequency oscillatory flow ventilation (HFOV) was tried.
Pneumomediastinum, deemed to be secondary to pneumothorax, was conservatively managed without drain insertion. Intravenous antibiotics and dobutamine were commenced for suspected sepsis and hypotension respectively. Echocardiogram showed small pericardial effusion and normal contractility. The multidisciplinary team consensus was to adopt a conservative approach. Parenteral nutrition commenced.
On day 5, CXR showed improvement. 2 non-bubbling drains were clamped and later removed. However, due to clinical deterioration and re-accumulation on days 5, 6, and 7, three other TTs were required, with subsequent improvement. A repeat echocardiogram demonstrated signs of pulmonary hypertension. Nitric oxide, dobutamine, and adrenaline were adjusted to allow pulmonary vascular circulation dilatation and reduce systemic vasoconstriction and echocardiogram findings improved.
Extracorporeal membrane oxygenation was not deemed suitable and conservative management continued. The 5 chest drains remained in situ with varying effectiveness. On day 10, dobutamine was stopped, nitric oxide was weaned off and HFOV was de-escalated to conventional ventilation at a peak pressure of 26 cmH2O and PEEP of 7 cmH2O. Only one drain bubbled continuously and then was removed on day 13.
Enteral feeding was started on the next day. Serial cranial ultrasounds showed no intraventricular hemorrhage or ischemic injury.
Laryngotracheobronchoscopy under general anesthetic identified no definite airway laceration, but erythema was seen at the carina which could indicate old injury (Fig. 3). By day 19, all chest drains were removed. He was extubated on day 24 and CXR appearances improved. He was discharged home on day 66.
Discussion
Due to high morbidity and mortality, awareness of the risk factors of neonatal pneumothorax is important. A birthweight of <2.5kg has a 10-times, and a 1-minute APGAR score of less than 7 has a 2.67-times increased risk of pneumothorax.[1] C-sections also increase the risk of neonatal pneumothorax. [2] These risk factors are relevant to our case.
The pneumothorax was suspected due to increased work of breathing, desaturation, and increased oxygen requirements and confirmed by transillumination and CXR. Transillumination is rapid but CXR is potentially associated with delayed management and harmful radiation.[1] Lung ultrasound (LUS) supersedes transillumination owing to a better diagnostic profile (Sensitivity: 96.7%, specificity: 100%) as it is rapid, repeatable, and detects even small non-tension pneumothorax. [1]
The literature review established different management techniques in neonates with pneumothorax and associated pneumoperitoneum. Conservative management is advised for nonsurgical pneumoperitoneum as it would resolve once the pneumothorax is managed. [3] Needle aspiration followed by TT is the emergency treatment for tension pneumothorax. A venous catheter, a 22-gauge cannula, connected to an underwater seal can also be used to drain a neonatal pneumothorax, reducing inpatient stay and surgical complications. [4] Due to persistent, very large pneumothorax, multidisciplinary and multi-center discussions occurred; he was considered unstable in the early stages for the CT scan. General anesthesia and bronchoscopy also carry potential risks and locating an airway injury can be challenging in such preterm or low birthweight infants. [5]
In patients with stable vital signs, absence of respiratory distress, less than 1cm tracheal laceration, and no sepsis, conservative management by placing the uncuffed tube distal to the injury is an option. [6] Aurilia et al. report successful treatment of significant pneumothorax with HFOV without TT in stable preterm infants. [7] Huseynov used an inexpensive blood patch safely to tape persistent air leaks in a newborn after 15 days of pneumothorax despite TT and continuous suctioning.[8] Other studies report using fibrin glue but with risks of hypercalcemia, diaphragmatic paralysis, localized tissue necrosis, and contralateral pneumothorax [9] or chemical agents, such as povidone-iodine, with unknown sequelae in children or significantly challenging selective bronchial intubation. [8] Surgical intervention is usually applied in unstable patients where bridging the defect is not feasible. Restino et al. describe a bedside emergency right thoracotomy and further dissection revealing an injury near the trachea bifurcation. Primary repair was undertaken with a chest tube left in place. [5]
Anticipating and preventing complications of pneumothorax is essential. Air leak raises intrathoracic pressure and decreases cardiac output, causing hypotension requiring inotropes, as in our case. Neurologically, up to 89% of very low birth-weight infants with air leaks resulting in hypotension are prone to grade 3 or 4 intraventricular hemorrhage secondary to cerebral ischemia at watershed zones.[10] Fortunately, this complication did not develop in our patient.
To summarize, pneumothorax is a life-threatening condition with potential iatrogenic causes. Massive air leak can extend to develop pneumomediastinum and pneumoperitoneum. Risk factors include prematurity, low birth weight, low APGAR scores, and C-section delivery. Therefore, very cautious airway instrumentation is required in neonates. The management is patient-specific. Pneumoperitoneum should not always warrant drains or exploratory laparotomy as nonsurgical pneumoperitoneum can occur in ventilated neonates and those with airway injury. Our case demonstrates the challenges of managing a massive air leak in a premature newborn. With adequate tube thoracocentesis and HFOV, he successfully recovered from presumed iatrogenic persistent pneumothorax and pneumoperitoneum.
Notes
n1Conflicts of interest. None.
n3Author contributions: Author(s) declared to fulfill authorship criteria as devised by ICMJE and approved the final version. Authorship declaration form, submitted by the author(s), is available with the editorial office.
n4Consent to Publication: Author(s) declared taking informed written consent for the publication of clinical photographs/material (if any used), from the legal guardian of the patient with an understanding that every effort will be made to conceal the identity of the patient, however it cannot be guaranteed.
References
|
|
| 1. |
Liu J, Kurepa D, Feletti F, Alonso-Ojembarrena A, Lovrenski J, Copetti R, et al. International expert consensus and recommendations for neonatal pneumothorax ultrasound diagnosis and ultrasound-guided thoracentesis procedure. J Visualised Exp. 2020. Available from: https://pubmed.ncbi.nlm.nih.gov/32225145/. |
| 2. |
Benterud T, Sandvik L, Lindemann R. Cesarean section is associated with more frequent pneumothorax and respiratory problems in the neonate. Acta Obstetricia et Gynecologica Scandinavica. 2010; 88:359–61. Available from: https://obgyn.onlinelibrary.wiley.com/doi/full/10.1080/00016340802668899. |
| 3. |
Gummalla P, Mundakel G, Agaronov M, Lee H. Pneumoperitoneum without intestinal perforation in a neonate: Case report and literature review. Case Rep Pediatr. 2017: 6907329. Available from: https://www.hindawi.com/journals/cripe/2017/6907329/.
|
| 4. |
Phuyal R, Basnet R, Sapkota A, Gautam U, Chikanbanjar KV. Pneumothorax in a preterm neonate: a case report. J Nepal Med Ass. 2021; 59:608–10. Available from: http://www.jnma.com.np/jnma/index.php/jnma/article/view/5819.
|
| 5. |
Restaino KM, Obermeyer RJ, Tsai KW. Surgical repair of an iatrogenic tracheal injury in a very low birth weight infant. J Pediatr Surg Case Rep. 2014; 2:104–6. Available from: https://www.sciencedirect.com/science/article/pii/S2213576614000220.
|
| 6. |
Kahvecioglu D, Alan S, Gollu G, Erdeve O, Atasay B, Cakmak M, et al. Conservative treatment of neonatal pneumomediastinum with subcutaneous emphysema due to airway injury. Ankara Universitesi Tip Fakultesi Mecmuasi. 2013; 66. Available from: https://cms.galenos.com.tr/Uploads/Article_18455/AUTFM-66-71-En.pdf.
|
| 7. |
Aurilia C, Ricci C, Tana M, Tirone C, Lio A, Gambacorta A, et al. Management of pneumothorax in hemodynamically stable preterm infants using high frequency oscillatory ventilation: report of five cases. Ital J Pediatr. 2017; 22:114. Available from: https://doi.org/10.1186/s13052-017-0436-y.
|
| 8. |
Huseynov M. A first case report of neonatal persistent pneumothorax treated with an autologous blood patch. Turk Pediatri Ars. 2020; 55:438-40. Available from https://pubmed.ncbi.nlm.nih.gov/33414664/.
|
| 9. |
Sarkar S, Hussain N, Herson V. Fibrin glue for persistent pneumothorax in neonates. J Perinatol. 2003; 23:82-4. Avi H, Koshizuka K, Matsumoto M. Perforation of Meckel's diverticulum manifesting as aseptic peritonitis in a neonate: Report of a case. Surg Today. 2007; 37:881-3.
|
| 10. |
Altamimi T, Read B, da Silva O, Bhattacharya S. Airway injury and pneumomediastinum associated with less invasive surfactant administration in a premature neonate: a case report. BMC Pediatrics. 2021; 21:500. Available from: https://pubmed.ncbi.nlm.nih.gov/34758781/.
|