Introduction
Anorectal malformation (ARM) and Hirschsprung's disease (HD) rarely co-occur. Although the exact frequency of this association is unknown, the coexistence of HD with ARM has been reported in 2.3-3.4 percent of cases. [1], [2], [3] Classic HD and ARM were usually documented. To the authors’ knowledge, no case of TCA with ARM have reported in the literature. We are reporting a case of a 3-day-old female with this unusual association.
Case Report
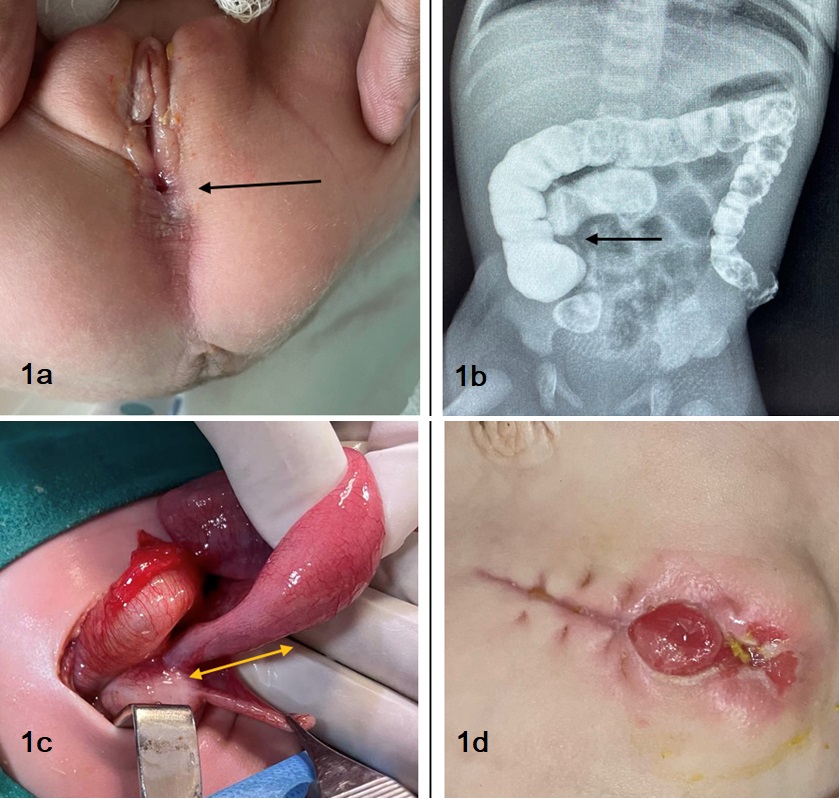
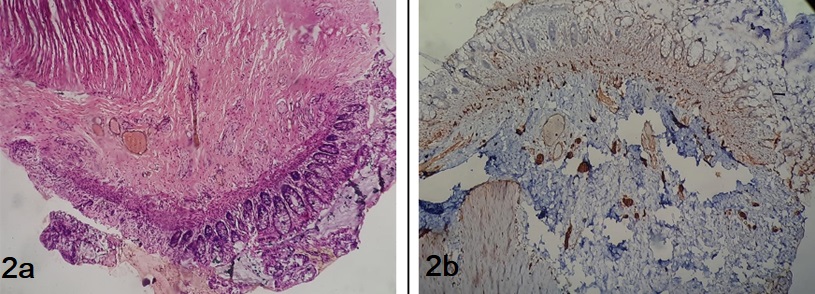
A 3-day-old female weighing 3.6 kg, first-born of a non-consanguineous marriage, full-term normal vaginal delivery, presented to the emergency department with failure to pass meconium since birth associated with progressive abdominal distension. She had a history of NICU admission for 2 days due to respiratory distress which was managed conservatively. The patient's vital signs were within normal limits, and her abdomen was significantly distended and tense on palpation, with absent bowel sounds. Upon examining the perineum, three openings were visualized, the rectal opening in the perineum just behind the posterior fourchette as a perineal fistula (Fig. 1a). A 10Fr infant feeding tube was inserted through the perineal fistula, and meconium was emptied with saline washouts, after which the abdominal girth decreased. The patient was hospitalized and treated with rectal washouts, intravenous antibiotics, and gradual dilation of the fistulous orifice. The patient was examined to rule out any other related anomalies, such as VACTERL, which were within normal limits. Because the patient did not respond well to conservative therapy, did not pass stool spontaneously, and had persistent abdominal distension, a high-divided sigmoid colostomy was performed on day 5 of her hospital stay. Intraoperatively, the sigmoid colon and rectum were found to be filled with thick meconium, with a normal caliber sigmoid colon, following which thorough proximal and distal bowel washes were performed. Despite proximal stoma washes and prokinetic medicines, the sigmoid colostomy stoma did not function postoperatively. Four days after surgery, a retrograde contrast study via the colostomy revealed a constriction in the distal ileum (Fig. 1b) with a normal caliber colon. On postoperative day 5, the patient was re-explored. Intraoperatively, there was a normal caliber colon with a 5cm transition zone discovered at the ileocaecal junction (Fig. 1c), after which a double barrel ileostomy (Fig. 1d) was performed. Multiple specimens were obtained from the distal ileum, transverse colon, and sigmoid colon and sent for histopathological evaluation (Fig. 2a,2b), which revealed absent ganglion cells and nerve bundle hypertrophy, giving rise to the diagnosis of TCA. The patient is doing fine postoperatively and waiting for the final definitive surgery.
Discussion
Pediatric surgery frequently encounters Hirschsprung disease and anorectal malformations, among other common congenital anomalies. However, the association between the two disorders is extremely uncommon, with relatively few documented cases (Table 1). Given that the incidence of ARM is predicted to be 1 per 3000 live births and that of HD is 1 per 5000 live births, we can anticipate an association of approximately 1 per 15000000. Patients with anorectal malformations are not regularly examined for Hirschsprung's disease since the coexistence of both disorders is exceptionally infrequent in the general population. [2] However, this combination is more common in patients with syndromic disorders such as Down syndrome, Pallister- Hall syndrome, Waardenburg- Shah syndrome, and Malrotation. [4], [5]
Following the correction of the anorectal malformation, the unusual coexistence of Hirschsprung's disease can have catastrophic results. As in the current case, patients who get a colostomy at an aganglionic segment as the initial treatment for anorectal malformation will not achieve bowel function. This should alert the likelihood of the existence of Hirschsprung's disease to the surgeon.
The treatment of this association is determined by the extent of the affected bowel, the location of the disease, and the initial treatment done for the ARM.[1] Because this association is diagnosed in stages, surgical corrections must be planned individually. Furthermore, the combined correction of HD and ARM poses a challenge. A review of the relevant literature showed that Soave's pull-through and the Duhamel procedure are the most common procedures done for HD after surgical correction of ARM. [1], [4], [6] But the management of TCA is different. TCA is treated by early decompression of the colon through an ostomy using the most distal ganglionated bowel in the neonatal period. This is usually followed by a second reconstructive procedure after the child has had enough time to grow and any concerns with nutrition, fluid, and electrolytes have been corrected. For the definitive treatment of TCA, multiple procedures have been described, such as Martin's ileo-colostomy (ileo-total colonic side-to-side stapled anastomosis), Boley's modification (only ascending colonic patch), and J pouch ileoanal anastomosis. [7], [8] In terms of perioperative morbidity, mortality, enterocolitis, and functional results, studies [7], [8] have shown there is no better surgical technique for treating TCA. The operational procedure used should be based on the center's and the surgeon's experience and expertise.
TCA has not been documented in association with ARM. To the best of our knowledge, our case with TCA coupled with perineal fistula will be the first case of this extremely unusual occurrence. Even though it is uncommon, the association of HD and ARM is something that needs to be taken into consideration in cases where functional issues continue to exist after ARM has been surgically corrected.
In conclusion, it is a very unusual occurrence for patients to have HD and ARM at the same time. The association of TCA and ARM is even rarer. A case of low ARM with fistula with persistent abdominal distension not responding to rectal washes and dilatation should raise a suspicion of Hirschsprung Disease and should be subjected to contrast enema to rule out this rare association.
Notes
n1Conflicts of interest. None.
n3Author contributions: Author(s) declared to fulfill authorship criteria as devised by ICMJE and approved the final version. Authorship declaration form, submitted by the author(s), is available with the editorial office.
n4Consent to Publication: Author(s) declared taking informed written consent for the publication of clinical photographs/material (if any used), from the legal guardian of the patient with an understanding that every effort will be made to conceal the identity of the patient, however it cannot be guaranteed.
References
|
|
| 1. |
Hofmann AD, Puri P. Association of Hirschsprung's disease and anorectal malformation: a systematic review. Pediatr Surg Int. 2013; 29:913-7. |
| 2. |
Nakamura H, Puri P. Concurrent Hirschsprung's disease and anorectal malformation: a systematic review. Pediatr Surg Int. 2020; 36:21-4. |
| 3. |
Raboei EH. Patients with anorectal malformation and Hirschsprung's disease. Eur J Pediatr Surg. 2009; 19:325-7.
|
| 4. |
Li MH, Eberhard M, Mudd P, Javia L, Zimmerman R, Khalek N, et al. Total colonic aganglionosis and imperforate anus in a severely affected infant with Pallister-Hall syndrome. Am J Med Genet A. 2015; 167a:617-20.
|
| 5. |
Stratulat-Chiriac I, Mc Laughlin D, Antao B. Rare association of extended total colonic aganglionosis and intestinal malrotation. J Neonatal Surg. 2020; 5:61.
|
| 6. |
Flageole H, Fecteau A, Laberge JM, Guttman FM. Hirschsprung's disease, imperforate anus, and Down's syndrome: a case report. J Pediatr Surg. 1996; 31:759-60.
|
| 7. |
Lamoshi A, Ham PB, Chen Z, Wilding G, Vali K. Timing of the definitive procedure and ileostomy closure for total colonic aganglionosis HD: Systematic review. J Pediatr Surg. 2020; 55:2366–70.
|
| 8. |
Levitt MA. Regarding the timing of the definitive procedure and ileostomy closure for total colonic aganglionosis HD: Systematic review. J Pediatr Surg. 2021; 56:1082.
|